
development of more discrete conduction system block. Further study is warranted to assess the potential differential impact of this therapy on QRS prolongation vs. Incident IVCD, but not BBB, is significantly reduced by losartan-based treatment. In a multivariable Cox model that adjusted for other statistically significant predictors of incident IVCD in this population (age, sex, race, history of ischemic heart disease, MI, heart failure, diabetes or atrial fibrillation, prior antihypertensive treatment, baseline total and HDL cholesterol, serum glucose and creatinine and baseline QRS duration as standard covariates and incident MI and on-treatment systolic and diastolic pressure, BMI and Cornell voltage as time-dependent covariates), losartan treatment remained associated with a 13% lower risk of new IVCD (hazard ratio 0.87, 95% CI 0.77-0.98, P = 0.021). In univariate Cox analyses, losartan-based treatment was not associated with a significantly reduced risk of either new LBBB (hazard ratio 0.95, 95% CI 0.79-1.14, P = 0.583) or RBBB (hazard ratio 1.02, 95% CI 0.76-1.36, P = 0.903), but resulted in a 15% lower risk of new IVCD (hazard ratio 0.85, 95% CI 0.76-0.95, P = 0.005). QRS duration and BBB were determined on in-study ECGs done at 6 months, 1 year and then yearly.ĭuring 4.8 ± 1.0 years follow-up, 459 patients developed new LBBB (5.5%), 184 (2.2) new RBBB and 1173 (16.5%) a new IVCD. Risk of incident intraventricular conduction delay (IVCD), defined as new QRS duration at least 110 ms was assessed in the 7110 patient subset who also had baseline QRS duration less than 110 ms. atenolol-based treatment was assessed in 8342 hypertensive patients without baseline RBBB or LBBB. Risk of new right (RBBB) or LBBB in relation to losartan-based vs. The relationship of incident conduction system disease to angiotensin receptor blocker therapy has not been examined.

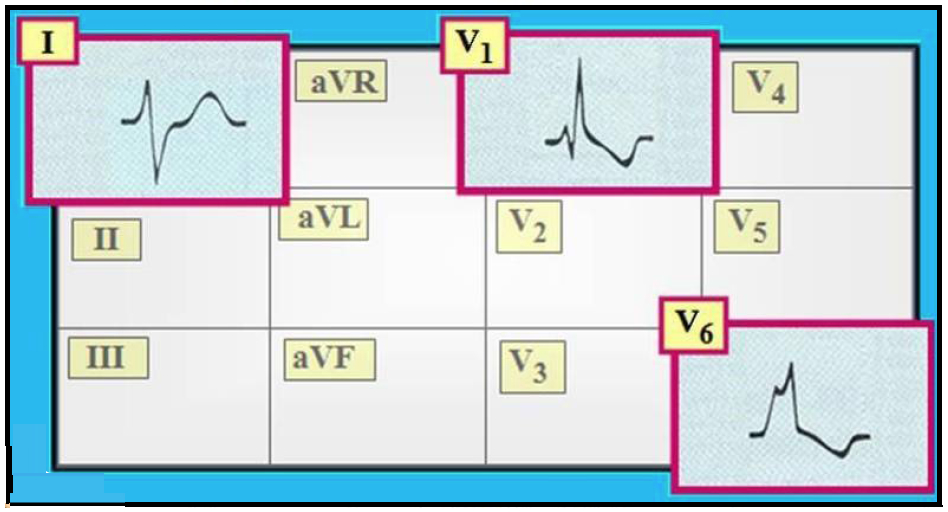
The distinction between RBBB and LBBB is simple, as illustrated in this figure. The hallmark of both RBBB and LBBB is the QRS duration which is by definitions 120 ms or longer. Note that the paper speed is 50 mm/s (1 large box equals 100 ms). Long Term (5yr) Outcome (Survival) in MADIT-CRT All patient groups benefit All with LBBB Goldenberg et al.NEJM 2014 370:1694-1701. Right bundle branch block (RBBB) and left bundle branch block (LBBB). All rights reserved.Previous work has demonstrated that treatment of hypertensive patients with the angiotensin-converting enzyme inhibitor lisinopril was associated with a reduced incidence of a composite conduction system disease endpoint and also left bundle branch block (LBBB) compared with chlorthalidone therapy. LBBB No LBBB (IVCD, RBBB) 1 V1 V6 Loss of septal Q. Scar burden, not QRS pattern, is independently associated with adverse clinical outcomes.Ĭardiac resynchronization Intraventricular conduction delay Ischemic cardiomyopathy Left bundle-branch block Scar burden.Ĭopyright © 2018 Heart Rhythm Society. IVCD is associated with greater scar burden than LBBB in ICM CRT-defibrillator recipients.
Scar burden but not QRS morphology was independently associated with these outcomes on multivariate analysis. During 39-month follow-up, IVCD was associated with shorter survival free from transplant/ventricular assist device and shorter time to first appropriate device shock. LVEF improved less in patients with IVCD vs LBBB, but only scar burden not QRS morphology or duration was associated with LVEF increase ≥5%. IVCD patients demonstrated less QRS narrowing with CRT than LBBB patients, even when excluding IVCD patients with QRS duration <150 ms. Nonspecific IVCD is associated with greater scar burden and narrower baseline QRS duration than LBBB. We compared scar burden QRS duration LVEF change risk of death, transplant, or ventricular assist device and risk of appropriate device shocks between LBBB and IVCD patients, using multivariable analyses to determine relative associations between QRS pattern vs scar burden and outcomes. We analyzed 393 consecutive ICM patients with left ventricular ejection fraction (LVEF) ≤35%, QRS duration >120 ms, and LBBB or nonspecific IVCD who underwent single-photon emission computed tomography myocardial perfusion imaging and CRT-defibrillator implant. The purpose of this study was to determine whether post-CRT outcome differences in patients with ischemic cardiomyopathy (ICM) relate to intrinsic QRS pattern and/or scar burden. Patients with nonspecific intraventricular conduction delay (IVCD) benefit less from cardiac resynchronization therapy (CRT) than patients with left bundle branch block (LBBB).


 0 kommentar(er)
0 kommentar(er)
